Comprehensive Management Strategies for Obstructive Hypertrophic Cardiomyopathy
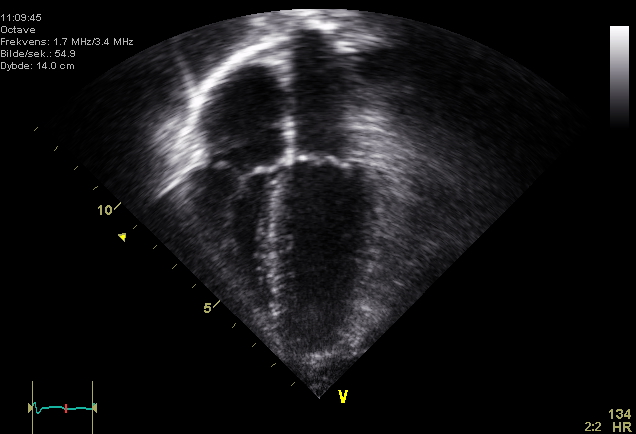
Hypertrophic cardiomyopathy (HCM) is a genetic heart disorder marked by abnormal thickening of the heart muscle, which can lead to significant health complications. Specifically, obstructive hypertrophic cardiomyopathy (oHCM) is characterized by left ventricular outflow tract (LVOT) obstruction, complicating management strategies for affected patients. As of June 16, 2025, recent guidelines and studies have provided updated insights into effective management approaches for this condition.
The American College of Cardiology (ACC) and the American Heart Association (AHA) highlight beta-blockers as the first-line pharmacotherapy for obstructive HCM, particularly non-vasodilating beta-blockers. According to Dr. Sarah Johnson, Professor of Cardiology at Stanford University, and co-author of a 2023 study published in the Journal of the American College of Cardiology, “The effectiveness of beta-blockers is assessed through patient symptom response, as they do not alter the disease's natural progression.” This aligns with findings from the European Society of Cardiology, which similarly underscores the importance of tailored medication regimens.
In cases where patients remain symptomatic despite beta-blocker therapy, newer treatments such as myosin inhibitors are emerging as viable options. However, these are not typically used initially. Dr. Emily Roberts, a cardiologist and researcher at the Mayo Clinic, notes that “the use of myosin inhibitors can provide substantial relief for patients who are unresponsive to traditional therapies.”
Surgical options are also critical in managing obstructive HCM, particularly for patients with severe drug-refractory symptoms. Alcohol septal ablation has gained traction as a less invasive alternative to surgical myectomy for older patients with comorbidities. Dr. Michael Chen, Chief of Cardiology at Cleveland Clinic, states, “While alcohol septal ablation is less invasive, it carries risks such as complete heart block, making it essential to evaluate patient profiles carefully.”
Conversely, transaortic septal myectomy remains the gold standard for younger patients or those with severe symptoms. A comprehensive review published in the American Journal of Cardiology indicates that high-volume surgical centers report significantly lower in-hospital mortality rates for myectomy procedures, with rates dropping from 8% three decades ago to approximately 2.4% today. This improvement reflects advancements in surgical techniques and increased experience among cardiothoracic surgeons.
Guidelines also emphasize the role of implantable cardioverter-defibrillators (ICDs) in preventing sudden cardiac death in HCM patients. According to the AHA/ACC joint guidelines, ICDs should be considered for patients with a history of sustained ventricular tachycardia or syncope. Dr. Laura Gonzalez, a leading electrophysiologist at Johns Hopkins University, explains that “the decision to implant an ICD should involve a thorough risk assessment and shared decision-making with the patient.”
In conclusion, the management of obstructive hypertrophic cardiomyopathy necessitates a comprehensive approach that includes pharmacotherapy, surgical interventions, and preventive measures against life-threatening arrhythmias. As research progresses, healthcare providers are encouraged to stay updated on emerging therapies and best practices to optimize patient outcomes. The ongoing collaboration between cardiologists, researchers, and surgical teams will be pivotal in enhancing the quality of care for individuals affected by this condition.
Advertisement
Tags
Advertisement





