Understanding Benign Dermoscopic Patterns: Insights from Dr. Orit Markowitz
In a recent interview with the Society of Dermatology Physician Assistants (SDPA), Dr. Orit Markowitz, a prominent dermatologist and Director of the Dermatology Residency Program at Mount Sinai Hospital, shared critical insights into the common misinterpretations of benign dermoscopic patterns. This discussion, which took place on June 1, 2025, emphasizes the importance of accurate dermoscopy for optimizing patient outcomes in dermatological care.
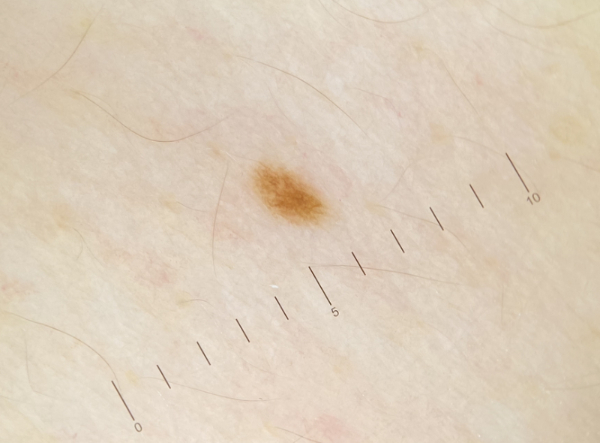
Dermoscopy, a non-invasive imaging technique, allows for enhanced visualization of skin lesions, aiding in the differentiation between benign and malignant conditions. Dr. Markowitz highlighted that many practitioners struggle with interpreting dermoscopic images due to a lack of training and experience, which can lead to misdiagnoses and unnecessary procedures. According to a 2023 study published in the Journal of the American Academy of Dermatology by Dr. Emily Choi, Assistant Professor of Dermatology at Stanford University, nearly 30% of benign lesions are misidentified as malignant in clinical settings, underscoring the need for improved educational resources for healthcare providers.
Dr. Markowitz pointed out several common dermoscopic patterns that are often misunderstood. For instance, the presence of a “network” pattern is frequently misinterpreted as indicative of malignancy. However, in many cases, it represents a benign condition, such as a common melanocytic nevus. This misinterpretation can lead to unnecessary biopsies and patient anxiety. "Training in dermoscopy is essential for accurate diagnosis and treatment planning, particularly in a field where visual cues are paramount," Dr. Markowitz stated during the interview.
The significance of dermoscopy extends beyond mere diagnosis; it plays a crucial role in preventive care. The American Academy of Dermatology (AAD) recommends regular skin checks and the use of dermoscopy as a standard practice for identifying skin cancer at its earliest stages. According to statistics from the Skin Cancer Foundation, one in five Americans will develop skin cancer in their lifetime, making early detection vital.
To address the educational gaps noted by Dr. Markowitz, organizations such as the AAD and the SDPA are investing in training programs aimed at enhancing the skills of dermatology practitioners. These initiatives include webinars, workshops, and certification courses focusing on dermoscopic techniques and pattern recognition.
Moreover, advancements in technology are aiding these educational efforts. Tools like the DermLite, a portable dermatoscope, are becoming standard in dermatology offices, allowing for immediate imaging and assessment of skin lesions. According to a report by the World Health Organization (WHO) published in 2024, the integration of such technologies in primary care settings can significantly reduce the incidence of skin cancer through improved diagnostic accuracy.
In conclusion, Dr. Markowitz’s insights underscore the importance of understanding benign dermoscopic patterns to enhance patient care in dermatology. As the field continues to evolve with technological advancements, ongoing education and training will be crucial for healthcare providers to ensure accurate diagnoses and effective treatment plans. The future of dermatology looks promising, with a focus on refining diagnostic techniques and improving patient outcomes through informed practice.
This interview serves as a reminder of the critical nature of accurate dermatological assessments and the need for continued professional development in interpreting dermoscopic images. As healthcare professionals strive for excellence in patient care, the insights shared by Dr. Markowitz will undoubtedly contribute to a more informed approach to dermatology.
Advertisement
Tags
Advertisement





